Cvs Copay

Pharmacy prior authorizations, quantity limits, specialty medications and step therapy for HealthChoice High, High Alternative, Basic and Basic Alternative Plans and High Deductible Health Plan (HDHP).n
Pharmacy prior authorization
nPharmacy prior authorization is a medical review that is required for coverage of certain medications such as those that:
- The copay for your monthly order will be charged only when your order is processed. You authorize CVS Pharmacy to charge your copay for each monthly order, up to a maximum of $200 If the amount exceeds $200, a technician or pharmacist will contact you for approval on the additional charges.
- Latuda Copay Savings Card: Eligible commercially insured patients may pay as little as $15 per prescription with savings up to $400 on each 30-day supply fill; for additional information contact the program at 855-552-8832. Applies to: Latuda Number of uses: 12 times within calendar year. More information please phone: 855-552-8832 Visit Website.
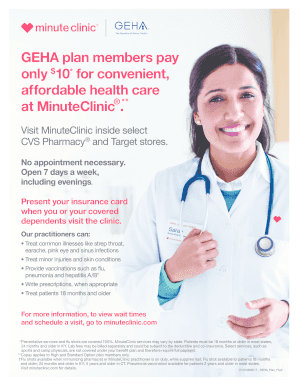
CVS does charge a delivery fee for prescriptions, but some health insurance plans may cover the fee, including Medicare Part D. (except for Kaiser and Medicaid) and your regular copay covers. Using telemedicine to see a doctor is a great option to help you take care of your health, while protecting yourself and others from the coronavirus. Learn more about Aetna's telehealth services for members during the COVID-19 pandemic, including benefits, copays, how to use, and more. $0 copay at in-network walk-in clinics, including MinuteClinic. Free CVS Pharmacy 1-2 day delivery on eligible Rx and select retail items 20% off select CVS Health-branded health and wellness products.
- n
- Are very high cost. n
- Have specific prescribing guidelines. n
- Are generally used for cosmetic purposes. n
- Have quantity limitations. n
Follow the steps below to request a prior authorization:
n- n
- Have your physician’s office call the pharmacy benefit manager toll-free at 800-294-5979. n
- The pharmacy benefit manager will assist your physician’s office with completing a prior authorization form. n
- If your prior authorization is approved, your physician’s office is notified of the approval within 24 to 48 hours. You are also notified in writing. n
- If your prior authorization is denied, your physician’s office is notified of the denial within 24 to 48 hours. You are also notified in writing. n
Types of prior authorizations
nTraditional prior authorization medications
nTraditional prior authorization reviews typically require that specific medical criteria be met before access to the medication is allowed.
Step therapy medications
nStep Therapy prior authorizations require you to first try a designated Preferred drug to treat your medical condition before the plan covers another drug for that same condition. Some step therapy medications may also be limited in quantity. If you require a step therapy exception, contact CVS Caremark Pharmacy Prior Authorization Department at 800-294-5979 or TTY 711.
Brand-name exception and non-preferred medication review
nA prior authorization for a brand-name or non-preferred drug may be approved when you are unable to tolerate the generic or preferred drug. All of these reviews follow the same process as described in the Pharmacy prior authorization section above.
Medications limited in quantity
nPharmacy prior authorizations, quantity limits, specialty medications and step therapy for HealthChoice High, High Alternative, Basic and Basic Alternative Plans and High Deductible Health Plan (HDHP).
Pharmacy prior authorization
Pharmacy prior authorization is a medical review that is required for coverage of certain medications such as those that:
- Are very high cost.
- Have specific prescribing guidelines.
- Are generally used for cosmetic purposes.
- Have quantity limitations.
Follow the steps below to request a prior authorization:
- Have your physician’s office call the pharmacy benefit manager toll-free at 800-294-5979.
- The pharmacy benefit manager will assist your physician’s office with completing a prior authorization form.
- If your prior authorization is approved, your physician’s office is notified of the approval within 24 to 48 hours. You are also notified in writing.
- If your prior authorization is denied, your physician’s office is notified of the denial within 24 to 48 hours. You are also notified in writing.
Types of prior authorizations
Traditional prior authorization medications
Traditional prior authorization reviews typically require that specific medical criteria be met before access to the medication is allowed.
Step therapy medications
Step Therapy prior authorizations require you to first try a designated Preferred drug to treat your medical condition before the plan covers another drug for that same condition. Some step therapy medications may also be limited in quantity. If you require a step therapy exception, contact CVS Caremark Pharmacy Prior Authorization Department at 800-294-5979 or TTY 711.
Brand-name exception and non-preferred medication review
A prior authorization for a brand-name or non-preferred drug may be approved when you are unable to tolerate the generic or preferred drug. All of these reviews follow the same process as described in the Pharmacy prior authorization section above.
Medications limited in quantity
Certain medications are limited in the quantity you can receive per copay based on their recommended duration of therapy and/or routine use.
If generics are available or become available for brand-name drugs that are limited in quantity, the generics are also limited in quantity. When new medications become available in drug categories that have quantity limits, they will automatically have quantity limits per copay. New drug categories also can become subject to quantity limits throughout the year.
Specialty medications
Specialty medications are usually high-cost medications that require special handling and extensive monitoring. You must pay a copay for each 30-day fill of a specialty medication. Copays are $100 for preferred medications and $200 for non-preferred medications.
TRS-Care Standard Prescription Drug Coverage
Working with your benefits plan sponsor, CVS Caremark provides convenient and flexible options for the prescription drugs you and your family may need. We are here to help you understand your plan so you can save time and money when it comes to your pharmacy benefits.
New Prescription Drug ID Cards for New TRS-Care Standard Participants
If you are new to TRS-Care and haven’t received your prescription drug ID card, register on this page under Member Sign In to print your personalized ID card. You can use this card at all network pharmacies.
Or you can print a general, temporary ID card without registering. Adding your personal details will allow you to use it at all network pharmacies until your permanent card arrives.
Check Drug Costs
The Check Drug Cost tool defaults to the most commonly dispensed quantity and day supply for each medication covered. You can modify the quantity and day supply totals when entering a medication for review.
How much will you pay? Find a drug cost based on your prescription dosage.
2021 Plan Year (Beginning Jan. 1, 2021)
2020 Plan Year (Beginning Jan. 1, 2020)
2021 Drug Lists and Other Information
Find a Pharmacy in Your Area
Network Retail Pharmacy Services
Participating network retail pharmacies will accept your TRS-Care Standard ID card and charge you the lesser of the negotiated CVS Caremark price or the usual and customary cost for up to a 31day supply of your prescription at a traditional retail network pharmacy, or up to a 90-day supply at a Retail-Plus network pharmacy. After your plan year deductible is met, you will pay the applicable copay* or coinsurance percentage of the price of the prescription until the out-of-pocket maximum is satisfied.
Your traditional retail pharmacy service is most convenient when you need a medication for a short period. For example, if you need an antibiotic to treat an infection, you can go to one of the many pharmacies that participate in the TRS-Care Standard program and get your medication on the same day. For your short-term prescriptions, you may save money by using pharmacies that participate in the Caremark network.
Retail-Plus Pharmacy Network
Retail pharmacies that choose to participate in the Retail-Plus network are able to dispense a 60-90 day supply of medication.
Mail Service through the Caremark Pharmacy
By using the CVS Caremark Mail Service Pharmacy, you can receive up to a 90-day supply of covered medications. After your plan year deductible is met, you will pay the applicable copay or coinsurance percentage of the price of the prescription until the out-of-pocket maximum is satisfied.
Cvs Copay Cards
The mail service pharmacy offers you convenience and potential cost savings. If you need medication on an ongoing or long-term basis, such as medication to treat asthma or diabetes, you can ask your doctor to prescribe up to a 90-day supply for home delivery, plus refills for up to one year.
*Copayment, copay or coinsurance means the amount a member is required to pay for a prescription in accordance with a Plan, which may be a deductible, a percentage of the prescription price, a fixed amount or other charge, with the balance, if any, paid by a Plan.
Cvs Copay Assistance For Specialty Drugs
Contact Customer Care
Prescription Copay Discount Cards
Customer Care for TRS-Care Standard Participants is available 24 hours a day, 7 days a week with your needs. 1-844-345-4577 option #1
